As we enter 2025, the workers’ compensation industry stands at the crossroads of innovation and adaptation. With advancements in generative AI (GenAI), a growing emphasis on holistic care, and an increasingly complex regulatory landscape, the challenges and opportunities for employers are more dynamic than ever.
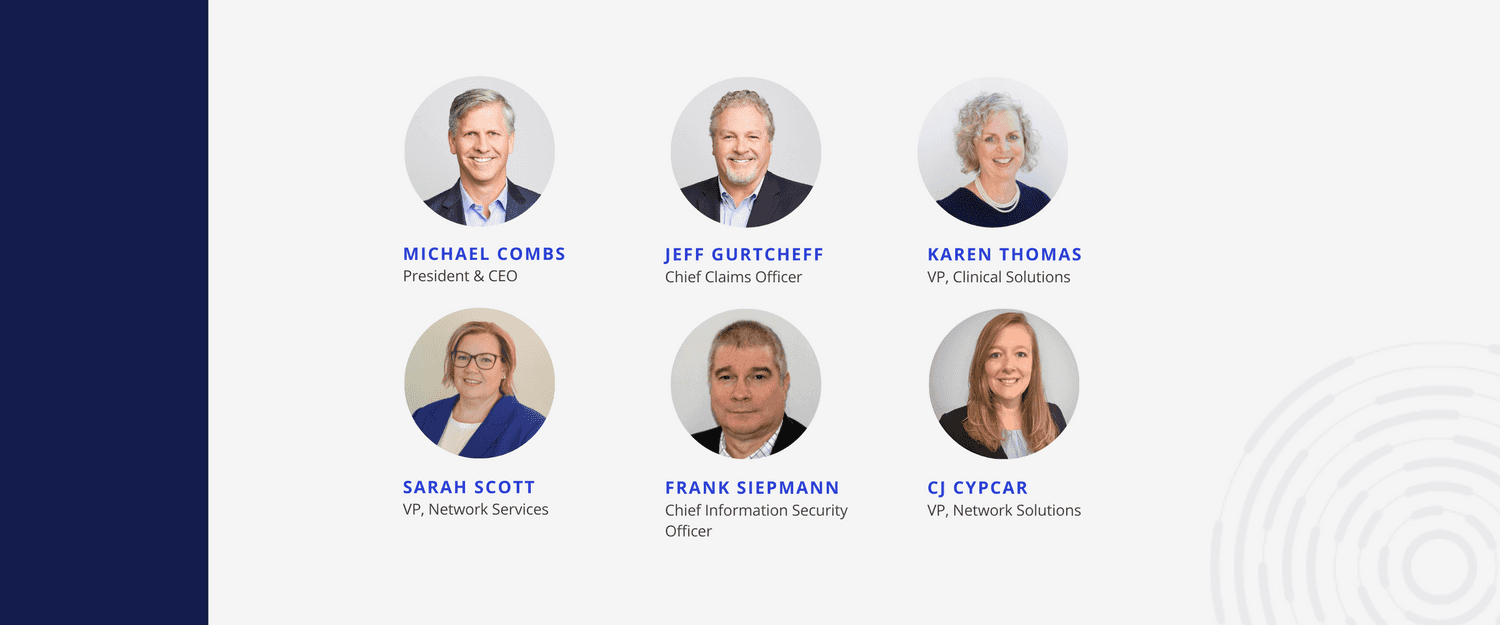
This year’s predictions from CorVel’s senior leaders shine a light on the key trends that will shape the future of workers’ compensation. Dive into our executives’ perspectives to discover how employers can meet the demands of today’s workforce while delivering better outcomes for injured workers.
AI Optimism Grows in Risk Management
Risk managers have traditionally approached emerging technology with caution, however, as advanced technology, notably generative AI, gains more use cases and measurable outcomes, attitudes are gradually shifting. While only 10% of risk professionals currently leverage GenAI for key processes, 48% plan to adopt GenAI-driven risk technology in the next three years. As leaders seek to leverage advanced predictive capabilities to uncover hidden trends and identify key outliers, we expect growth in enterprise-level GenAI adoption and implementation in 2025. For GenAI solution providers, offering risk managers adaptable yet efficient technologies with proven ROI will be key to long-term adoption. — Michael Combs, President & CEO
Stricter Regulations Offer More Structure
“2025 will be a pivotal year for claims management, driven by advancements in technology and its impact on risk management professionals. The adoption of artificial intelligence (AI) and other emerging technologies will create a need for talent skilled in deploying these tools across claims processes. However, the human touch remains critical in claims management—especially in maintaining the empathy necessary for effective communication between adjusters and injured workers. This “high-tech, high-touch” approach will be critical to deploying a successful workers’ compensation program in 2025. Despite these technological advancements, the risk management talent pool will shrink unless leaders make intentional efforts to foster a pipeline of professionals who understand both the technological and human aspects of claims management. As demand for experienced talent grows in the industry, so will wage inflation and Average Weekly Wages (AWW), particularly at the state level. As states grapple with the labor market, they will also focus on redefining legislation around mental health claims and presumptions for diseases, illnesses, and viruses in a post-pandemic world. Many states will begin to consider these conditions as primary injuries—not just for first responders—but for all workers, recognizing them as compensable.” — Jeff Gurtcheff, Chief Claims Officer
Cyber Upskilling Critical for AI Innovation
Across industries, the power of AI to drive efficiencies and improve outcomes is growing, with 61% of top business leaders planning to increase generative AI investments in the next three years, according to KPMG. However, as new GenAI-driven tools and applications add complexity to organizations’ technical load, companies must address the accompanying cyber risks. For workers’ compensation and insurance companies, securing both internal and customer-facing AI applications is critical as these tools may involve sensitive patient information and medical data from worker injury claims. With nearly 40% of IT leaders reporting key skills gaps in AI cyber-risk detection, a top priority of 2025 will be equipping security teams with the skills needed to secure AI applications and combat AI-driven cyberattacks. — Frank Siepmann, Chief Information Security Officer
Mental Health as a Standalone
According to Mercer, 94% of large employers have strengthened mental health support, and about two-thirds (68%) have added or enhanced employee assistance programs focused on mental wellness over the last four years. This trend extends to revamped return-to-work programs as employers recognize the strong link between better mental well-being and faster physical recovery. In 2024, state-level jurisdiction took worker mental health support even further with legislative efforts, such as South Carolina’s proposed H.B. 4992 or Pennsylvania’s H.B. 1632, that support mental injury claims for first responders. While the validity of a mental injury (i.e., “mental-mental” claims) was previously contested, this shift reflects an industry-wide transformation in workers’ compensation. With advancements such as virtual reality treatment for trauma-induced psychological injuries and expanded telehealth options for long-term therapy on the rise, 2025 will see employers leveraging technology for more cost-effective, long-term mental health support. — Karen Thomas, Vice President, Clinical Solutions
Rising Costs Meet Rate Cuts
Driven by rising prescription drug costs and inflationary pressures, PwC estimates that medical cost growth will reach record levels in 2025, with an 8% cost trend. Annual federal regulation changes, such as CMS’s 2025 Medicare payment rule, could help mitigate these rising costs through strategic payment reductions aimed at fostering a more affordable healthcare system. However, states that rely on Medicare-based methodologies for workers’ compensation programs will need to strike a balance between rate reductions and maintaining a quality provider network focused on outcomes and return-to-work goals. In light of these changes, employers can support providers in treating injured workers by optimizing bill review processes and ensuring prompt and accurate payments. — CJ Cypcar, Vice President, Network Solutions Product Manager
A Promising Future for Value-Based Care
Following CMS’s 2021 announcement to transition Medicare and Medicaid beneficiaries to accountable care arrangements by 2030, provider adoption of alternative payment models has been slow due to financial and operational challenges. However, spurred by the rapidly evolving patient landscape, the past year saw increased adoption of value-based care to meet the need for more holistic, patient-centered healthcare delivery, with 93.5 million Americans currently in an accountable care arrangement. As the focus on improving access to high-quality care grows, 2025 will mark an inflection point for value-based care models to become more prevalent in workers’ compensation managed care. This shift away from fee-based models will be further supported by outdated fee schedules and insufficient reimbursement rates. Lastly, employer support for value-based care will also increase as companies seek long-term strategies to optimize treatment and recovery outcomes for injured workers. — Sarah Scott, Vice President, Network Services
From securing AI-driven tools to managing rising medical costs, embracing value-based care models, and expanding mental health support, the above insights underscore the critical shifts necessary to thrive in a transforming industry.
By adopting a proactive approach and remaining flexible to change, organizations can create a more resilient workers’ compensation ecosystem that drives efficiency, improves outcomes, and empowers employees.
Related Articles
Ready to get started?
Our team is ready to answer any questions and help you find the right solutions.