Claims Management Platform
CareMC: Built for Performance. Built by Expertise.
Claims management has never been easier with CareMC, which leverages best-in-class technology to deliver greater transparency, help employees recover more quickly, and maximize savings. With nearly 40 years of experience, we’ve enhanced claims management so professionals outrun risk and get ahead of costs.

Why CareMC?
One integrated platform for all claims management solutions.
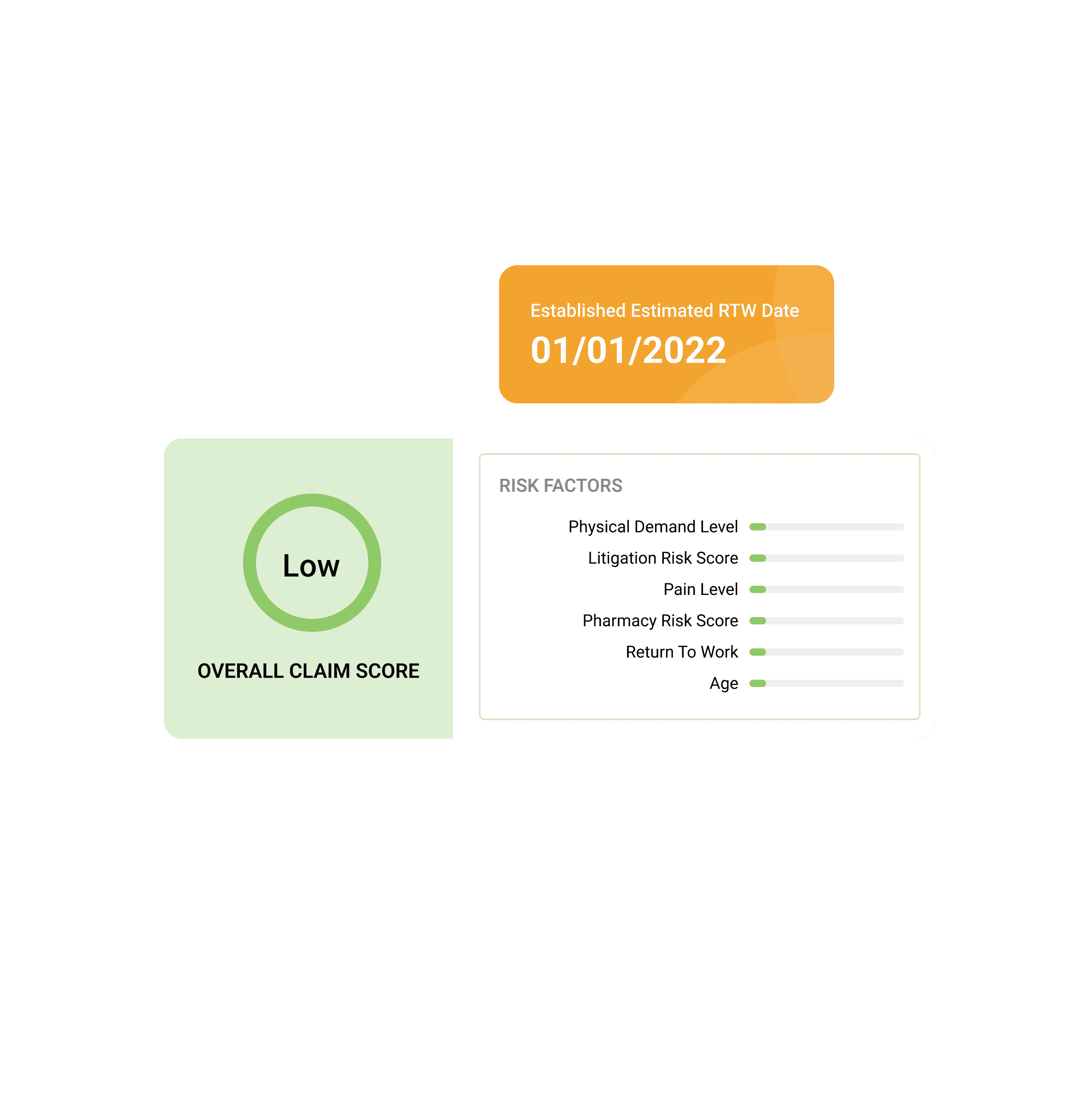
Get a personalized risk assessment.
- We use advanced technology to rate all data elements on a claim and grade its level of risk.
- Several factors such as return-to-work estimates, physical demand requirements, pain levels, and more are incorporated to conduct an accurate evaluation.
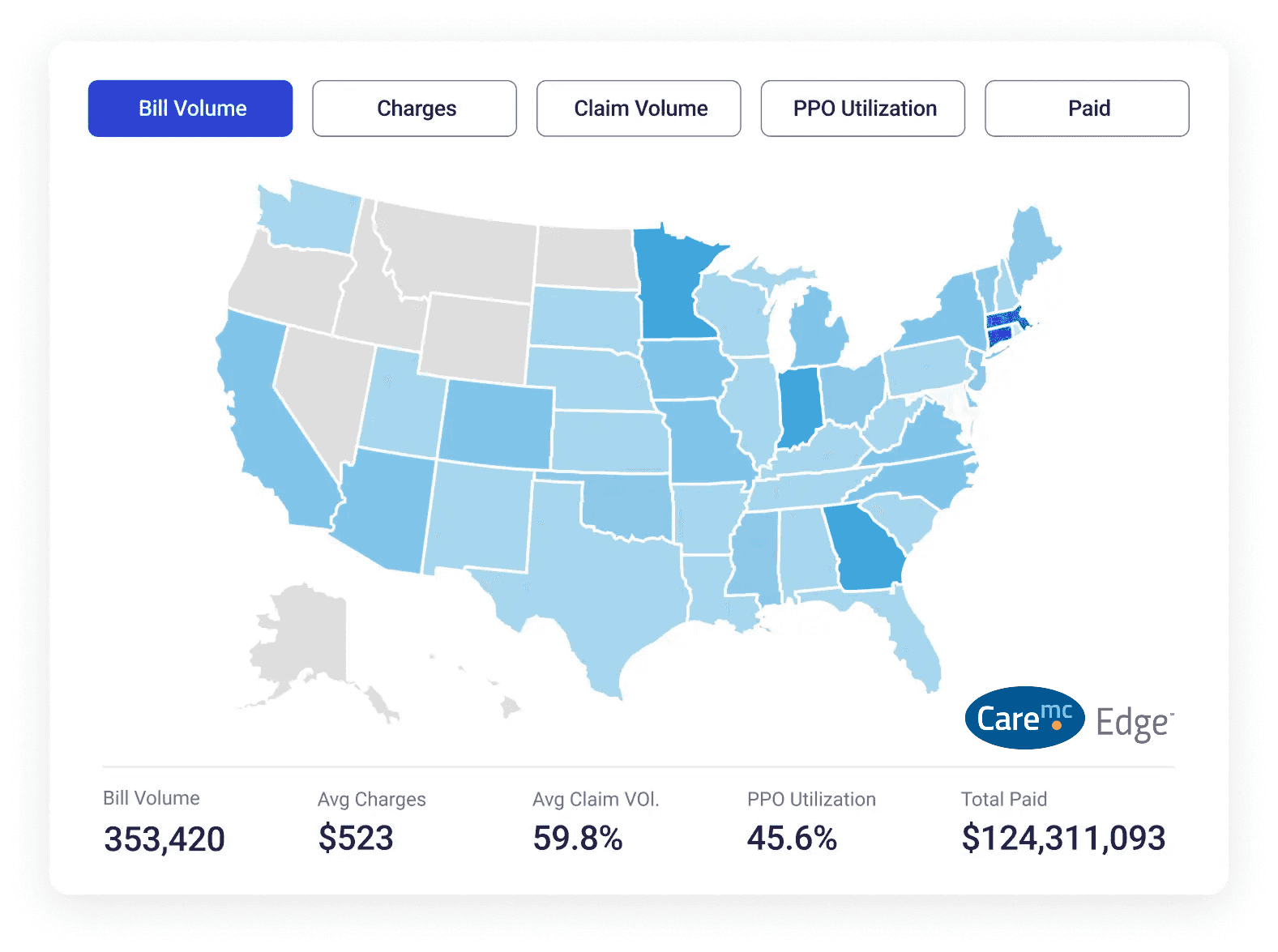
Manage everything, all from one place.
- Dynamic and interactive high-level overview of your entire program, delivering essential claims data and next steps through the entire process.
- Actionable insights for adjusters, period-over-period benchmarking, litigation information, and more.
- Complete visibility and real-time information through every stage to keep return-to-work progress on track.
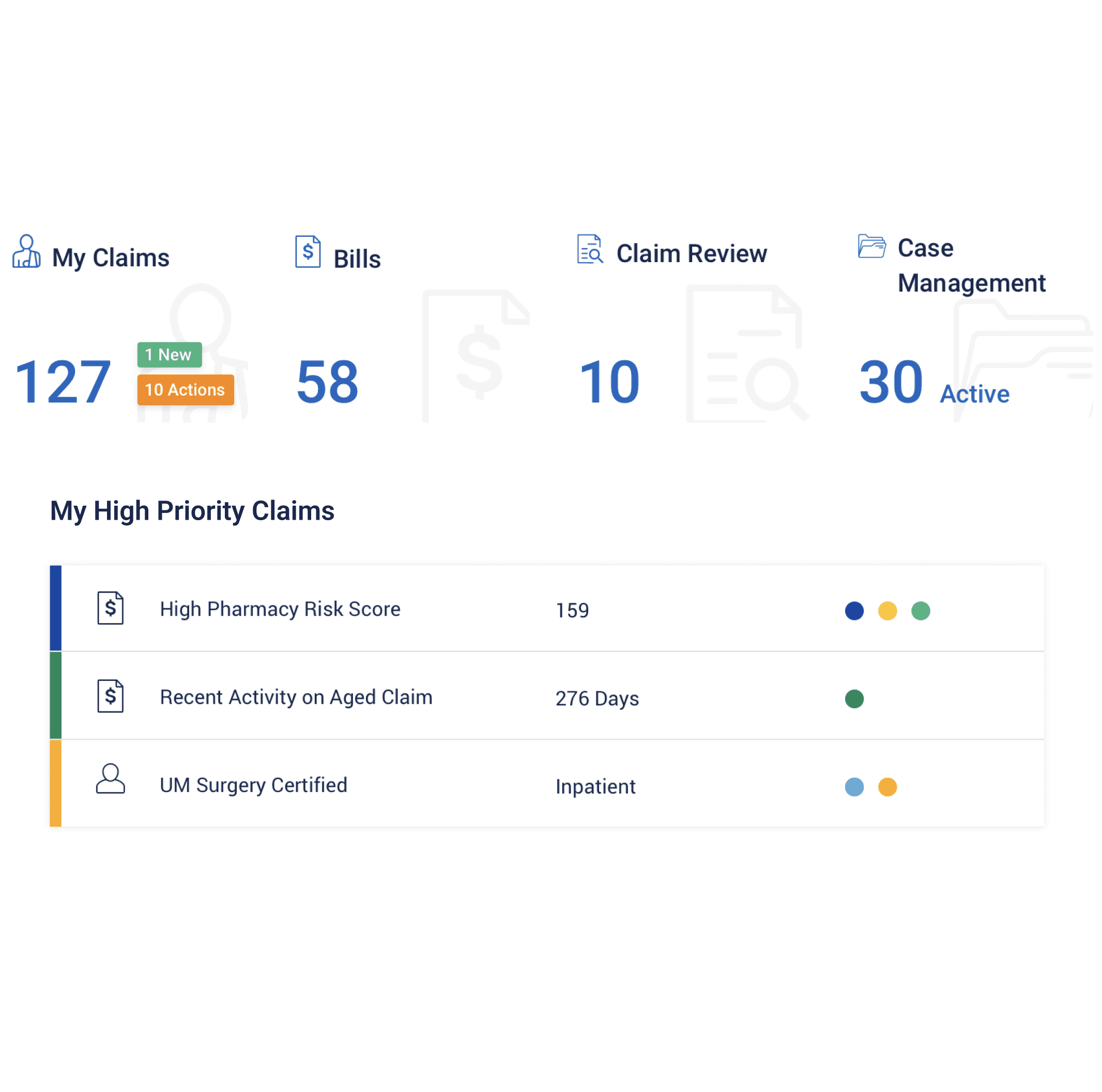
Ensure employees access quality care.
- Ongoing access to resources for case managers to proactively guide injured workers and deliver high-quality care.
- Predictive modeling for identifying potential barriers to recovery.
- A direct line to providers for immediate scheduling with specialty networks to ensure holistic recovery.
- Provides insights into pharmacy management of drugs and treatments.
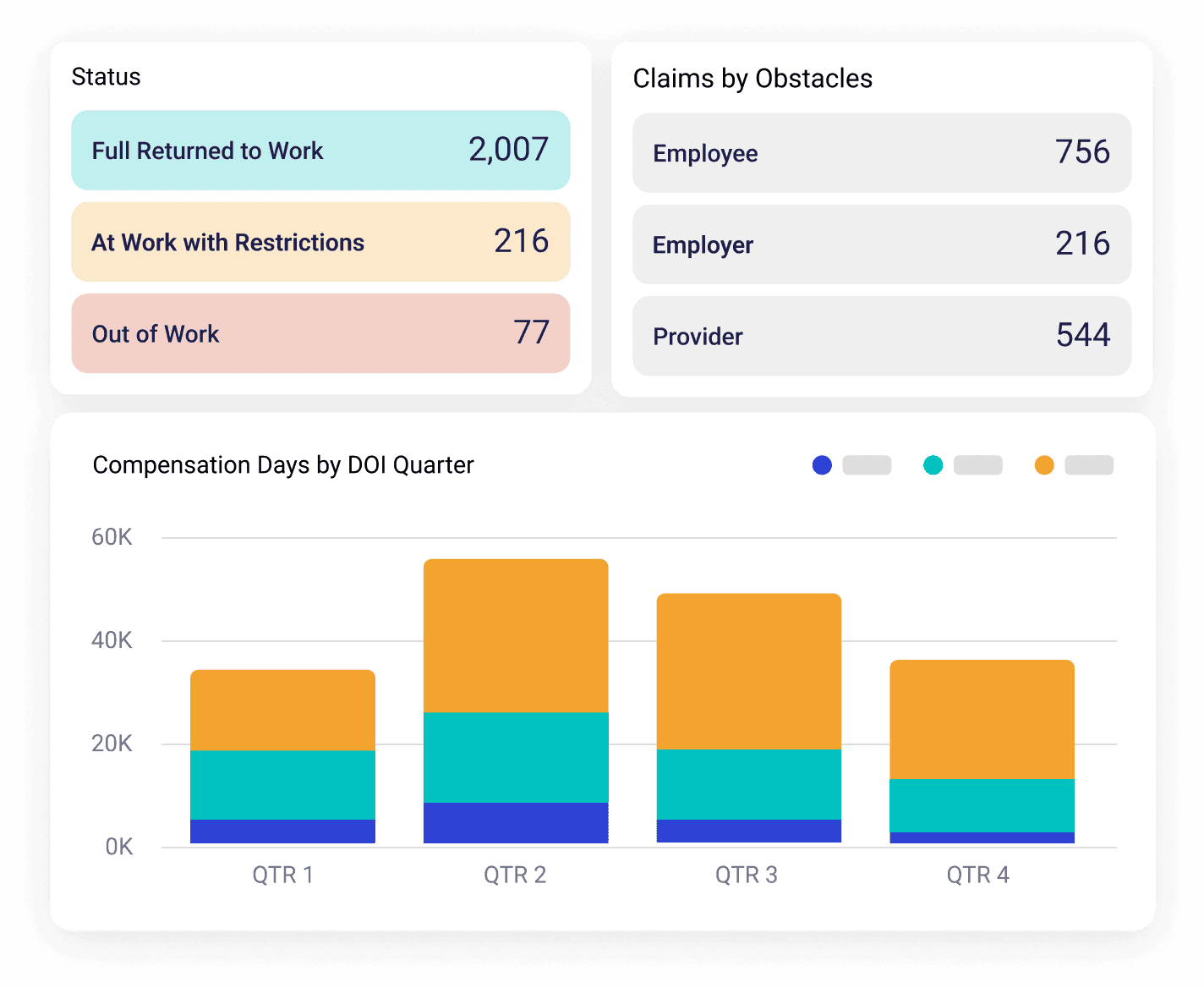
Take informed action to drive better outcomes.
- Comprehensive overview provides key details related to return-to-work plans, including work restrictions, dates, claim-specific notes, and status.
- Track the progress of return-to-work initiatives and monitor employees’ transition back to functional work positions.
- Visualize return-to-work journeys for optimized resource allocation and proactive management.
Generative AI Integration

Built For Results
CareMC is more than a claims platform. It’s the technology that supports people, process, and performance—delivering measurable results, not just automation.
CareMC is also the system that drives CorVel’s Operational Excellence (OpEx) Program. With real-time visibility into performance, integrated workflows, and embedded quality controls, CareMC ensures every claim is managed consistently and with care. It empowers claims teams to work smarter and stay aligned with program goals, compliance requirements, and injured worker needs.
- Real-Time KPIs & Dashboards: Tracks team and individual performance across quality, compliance, and resolution metrics.
- Smart Alerts & QA Triggers: Identifies documentation gaps, medical red flags, or workflow delays before they impact outcomes.
- Supervisor Oversight: Claims Supervisors have access to performance dashboards and quality indicators, enabling proactive coaching and intervention.
- Integrated Return-to-Work Tracking: Visualizes treatment timelines, recovery progress, and provider performance in one place.
CareMC powers CorVel’s high-performance culture—driving faster resolutions, smarter decisions, and more consistent outcomes across the board.
Learn more about how CareMC can help you manage claims and reduce costs.
Helpful Insights
View MoreRe-Engineering the Workers’ Comp Process to Improve Outcomes
Read More
CorVel Releases the New Integrated Claims Risk Score for Workers’ Compensation Claims, Leveraging Artificial Intelligence and Predictive Analytics
Read MoreFostering the Next Generation of Insurance with a Culture of Innovation and Technology
Read MoreReady to get started?
Our team is ready to answer any questions and help you find the right solutions.