Workers' Comp Claims Management
Getting people back to health & business back on track.


Navigating workers’ compensation can be difficult. We’re here to help.

Simplifying processes
Manage the entire claims process on our integrated platform, CareMC Edge, to streamline communication and increase efficiency.
Putting patient care first
We ensure that care is quality, consistent, and holistic with our patient advocacy model, comprehensive provider network, and virtual care options.
Optimizing savings
We prioritize putting injured workers’ care first in order to improve return-to-work rates, which in turn reduces inefficiencies and maximizes your savings.
People-centered & results-driven.
0%
Reduction in indemnity costs
0%
Decrease in medical spend
0%
Return-to-work rates for overall case
CareMC Edge
A single-source claims solution to improve efficiency and reduce costs.
With CareMC, the only fully integrated claims system in the industry, claims management will never be the same. CareMC leverages best-in-class technology to provide greater transparency, help employees recover more quickly, and reduce losses.
Learn More
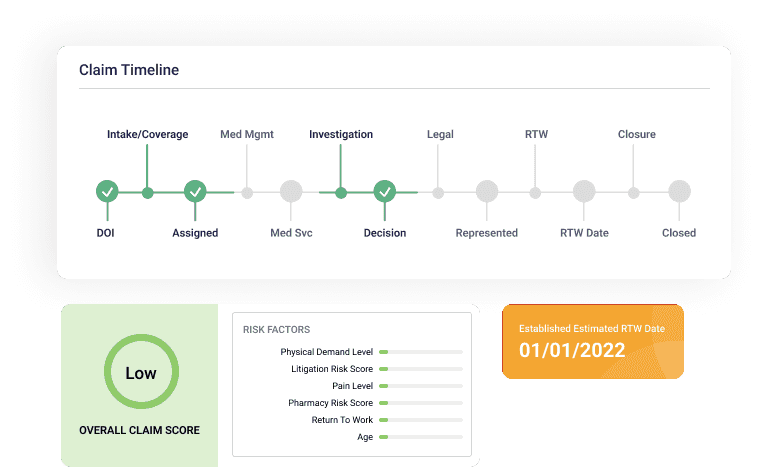
Personalized Claims Scores
Provide better care with individualized claims scores based on an employee’s medical history, pain levels, and other data points.
Greater Visibility for Clients
Eliminate costly delays in care and communication—we keep your data in one place and provide real-time information you can access anytime.
Expert Support
Get help from a team of risk management experts who will continually provide insight and work with you to ensure your solution fits your needs.
End-to-end workers’ compensation solutions.
Advocacy 24/7
Get immediate help when a workplace injury happens by calling our nurse triage hotline for intervention.
Learn More
Virtual Care
Reduce recovery time and claim costs by giving employees convenient access to care via telehealth.
Learn More
Case Management
Get expert help from case managers who advocate for employees and help optimize the claims process.
Learn More
Preferred Provider Network
Access the most comprehensive coverage available on the market at a discounted rate.
Learn More
Bill Review
Optimize savings and ensure accuracy with our AI technology and clinical expertise.
Learn More
Pharmacy Benefit Management
Reduce spend and improve patient safety with our high-touch model and 100% visibility into data.
Learn More
Ready to get started?
Our team is ready to answer any questions and help you find the right solutions.
